How to Increase Sperm Count Naturally: Root Causes + What to Do
Sperm count is declining.
Over the past several decades sperm counts have dropped by more than 50%, and the rate of decline has doubled since 2000.
Despite this, male fertility is still often overlooked.
About half of infertility cases involve male factors, yet evaluation and treatment tend to focus more heavily on women.
This can be frustrating, especially if you’re trying to conceive and still struggling without clear answers.
In this article, we’ll share what actually impacts sperm count and how to support it naturally.
Why Sperm Count Matters
Sperm count plays a direct role in the chances of natural conception.
For pregnancy to occur, sperm have to survive the vaginal environment, move through thick cervical mucus (the equivalent distance of 30 miles for a human!), and reach the egg.
A higher sperm count increases the likelihood that at least one sperm successfully completes that process.
But sperm count isn't just a fertility metric.
Hormones, blood sugar, inflammation, and nutrient status all influence sperm production. Fertility reflects how well your body is functioning overall.
What is a Normal Sperm Count?
Many experts consider the following ranges:
- Below 15 million/mL: Low
- 15–40 million/mL: Normal, but may still limit fertility
- 40+ million/mL: More supportive of optimal fertility
A “normal” sperm count is typically defined as 15 million sperm per milliliter or higher, based on World Health Organization (WHO)
reference ranges.
But the “normal” reference range is based on population averages, not ideal fertility outcomes.
Low-normal counts of 15-40 million/mL often come with weaker swimmers or odd shapes.
Aiming for at least 40 million sperm per ml of semen gives you much better odds of conceiving.
The 6 Root Causes of Low Sperm Count
1. Hormone Imbalances (Low Testosterone, High Estrogen, Thyroid Dysfunction)
Your brain and testicles communicate through a system called the HPG axis.
Here's how it works:
- The hypothalamus signals the pituitary with GnRH
- The pituitary releases LH (which supports testosterone production) and FSH (which supports sperm production)
- The testes respond by producing testosterone and sperm
When that signaling is disrupted, sperm production can decline.
Low testosterone reduces the support needed for sperm development in Sertoli cells, which can lower sperm count.
High estrogen
can also interfere with this system. High estrogen sends feedback to the brain, suppressing the signals that stimulate testosterone and sperm production.
Thyroid dysfunction also plays an important role. When thyroid function is low, sperm production can slow down significantly, even if other labs appear normal.
2. Blood Sugar Instability & Insulin Resistance
Blood sugar and insulin play a direct role in testosterone and sperm production.
When blood sugar is elevated or insulin resistance is present, testosterone can decline and oxidative stress can increase, both of which can negatively impact sperm production and sperm quality.
This can lead to:
- Reduced testosterone production (research shows 20-50% reductions)
- Increased oxidative stress, which can damage sperm DNA
- Impaired sperm development
3. Chronic Inflammation
Chronic inflammation can negatively impact both sperm production and quality.
Gut health can be a major contributor, influencing both inflammation and nutrient absorption:
- Leaky gut allows bacterial toxins (endotoxins) into your bloodstream, which can lower sperm production via the gut-testes axis
- Poor gut health impairs nutrient absorption, starving your body of important nutrients even if you eat them
- Gut bacteria imbalances increase oxidative stress, decreasing sperm production and worsening sperm quality

4. Nutrient Deficiencies That Sabotage Sperm
Without key nutrients, your body can struggle to produce enough sperm.
Here are a few deficiencies we see that increase the risk of low sperm count:
5. Environmental Toxins & Endocrine Disruptors
Certain environmental exposures can interfere with sperm production by disrupting hormones or increasing oxidative stress.
Endocrine-disrupting chemicals
like BPA, phthalates, and microplastics hide in plastics, food packaging, and water bottles. They mimic estrogen, confusing your HPG axis and reducing natural testosterone signals needed for sperm production.
Heat exposure also plays a role. The testes are designed to stay slightly cooler than body temperature to support sperm development. Regular exposure to heat, such as
hot tubs, saunas, tight clothing, or laptops on your lap, can significantly reduce sperm production.
Phone exposure is less clear.
Research on phone radiation and sperm health is mixed. Some studies suggest it may increase oxidative stress and DNA damage (from EMFs, heat, or both). A simple precaution is to carry it in a bag or back pocket, especially if it is there for long periods of time (4+ hours).
Occupational exposures can have a big impact. Regular contact with pesticides, heavy metals, solvents, or fumes can affect hormone balance and sperm quality.
6. Testosterone Therapy (TRT)
Testosterone therapy is a common but often overlooked cause of low sperm count.
When you take testosterone from an external source, your body reduces its own hormone signaling, which lowers the signals needed for sperm production.
This can lead to:
- Decreased sperm count, often to very low levels
- Reduced semen volume
- Changes in sperm motility and shape
- Testicular shrinkage over time
Fertility can sometimes recover after stopping TRT, but it takes time and is typically not immediate.
Recovery often takes3–12 months, and sometimes longer. Longer-term use can make recovery more difficult and, in some cases, not possible.
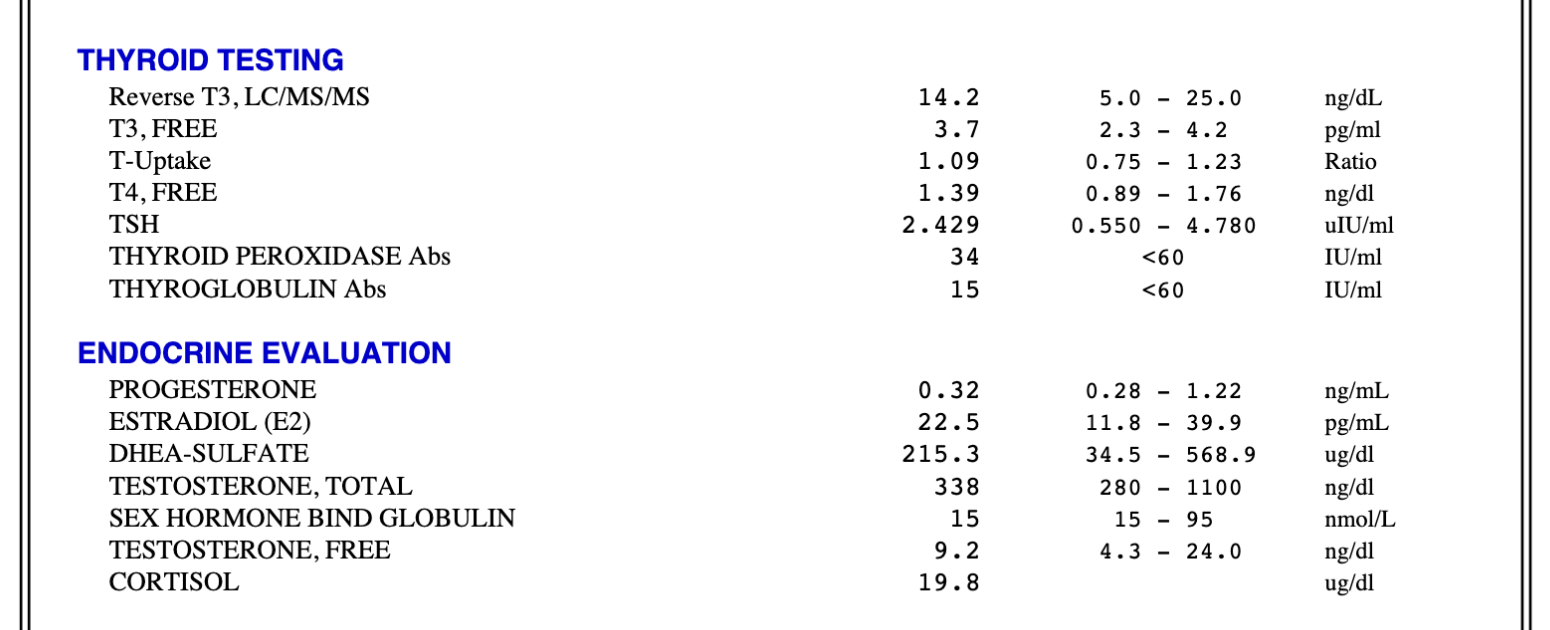
Stop Guessing: How to Identify What Is Affecting Sperm Count
Most men trying to increase their sperm count are guessing.
We often see men who have tried supplements or diet changes for months without improvement because they aren’t targeting what is actually driving the issue.
Testing allows you to identify what is impacting sperm production so you can take a targeted approach.
We recommend starting with a semen analysis to assess:
- Sperm count
- Motility
- Morphology
This can be done through a fertility clinic or at home. We often recommend Proov’s at-home test, which is more affordable than most clinic options, 97% accurate, and HSA/FSA eligible:
https://proovtest.com/PLATEANDCANVAS (use code PLATEANDCANVAS for 15% off)
If sperm count is low (or other abnormalities are present), the next step is evaluating potential root causes.
This may include:
- Hormones: total and free testosterone, LH, FSH, estradiol, prolactin, SHBG
- Metabolic health: glucose, fasting insulin, A1c
- Thyroid function: TSH, free T4, free T3, reverse T3, TPO Ab, TG Ab
- Nutrients: Vitamin D, zinc, vitamin A, iron
- Inflammation markers: homocysteine, CRP
How to Increase Sperm Count Naturally (Step-by-Step Plan)
Improving sperm count is not about one supplement or quick fix.
Here’s how to approach it.
Step 1: Stabilize Blood Sugar and Improve Metabolic Health
Blood sugar and insulin play a direct role in testosterone and sperm production.
Insulin resistance can lower testosterone and increase inflammation, both of which can impair sperm quality.
Focus on:
- Building balanced meals with the right ratios of protein, healthy fats, and fiber
- Strength training 3–4 times per week (muscle increases insulin sensitivity)
- Prioritizing 7-8 hours of sleep per night
Intermittent fasting can be helpful for some, but it is not appropriate for everyone. In some cases it can negatively impact fertility, which is why we approach it on a case-by-case basis.

Step 2: Reduce Inflammation
Chronic inflammation can lower testosterone and reduce sperm production. It can also damage developing sperm cells and increase the likelihood of sperm death.
Focus on:
- Increasing omega-3 intake and limiting excess omega-6 intake
- Prioritizing antioxidant-rich foods to combat oxidative stress
- Addressing gut health when indicated, as it can be a major source of inflammation
Step 3: Optimize Hormones Naturally
Sperm production depends on healthy hormone signaling. Low testosterone, elevated estrogen, or thyroid dysfunction can all affect sperm count.
Focus on:
- Eating enough healthy fats and carbohydrates to support hormone production (low-fat and low-carb diets can negatively impact testosterone)
- Reducing excess body fat (just a 5-10% weight loss can increase sperm count by 15-20%)
- Supporting thyroid function, which is essential for both testosterone and sperm production
Step 4: Replete Key Nutrients
Your body needs specific nutrients to produce healthy sperm. Deficiencies in nutrients like zinc, selenium, and folate can limit both sperm count and quality.
Focus on:
- Prioritizing nutrient-dense foods
- Testing to identify deficiencies
- Using targeted supplementation, rather than guessing (unnecessary supplements can disrupt nutrient balance)
Step 5: Reduce Toxin Load
Exposure to hormone-disrupting chemicals can interfere with hormone balance and sperm development.
This isn't about perfection. It's about making small changes where you can. They add up!
Focus on:
- Using glass or stainless steel instead of plastic when possible
- Filtering your drinking water (not all filters remove contaminants equally)
- Choosing safer personal care products (focus on the highest-impact products)

How Long Does It Take to Increase Sperm Count?
Sperm production takes time.
It takes about 70–90 days to produce new sperm, which means changes you make today will not show up immediately.
Most men need at least 3 months to see improvements. In some cases, it can take longer depending on what is driving the issue.
This is why quick fixes fall short. Improving sperm count requires consistency and addressing the underlying factors.
Bringing It All Together
Improving sperm count is about creating an environment in your body that supports healthy sperm production. Hormones, metabolism, inflammation, nutrient status, and environmental exposures all play a role.
This is why many men try different strategies without seeing results. Without identifying what is actually driving the issue, it becomes guesswork.
When the underlying factors are addressed, improvements are often possible.
If you want personalized strategies, we take a root-cause, testing-based approach to help identify what is impacting your fertility and build a plan around it.
You can book a discovery call here to see if it is a good fit.
Continue Reading